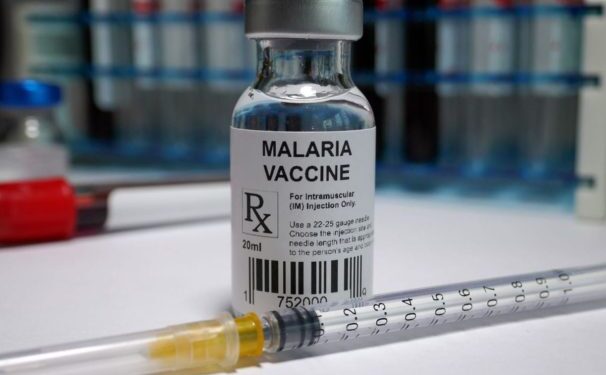
A keenly-watched Oxford’s malaria vaccine has secured its first approval, in Ghana, as the African country ramps up efforts to combat the mosquito-borne disease that kills a child every minute.
The effort is one of several focused on addressing the disease that kills over 600,000 each year, most of them children in Africa.
The complicated structure and lifecycle of the malaria parasite has long stymied efforts to develop vaccines.
After decades of work, the first malaria vaccine, Mosquirix from British drugmaker GSK, was last year endorsed by the World Health Organization (WHO), but a lack of funding and commercial potential has thwarted the company’s capacity to produce as many doses as needed.
The Oxford vaccine, which has secured regulatory approval in the age group at the highest risk of death from malaria – children aged 5 months to 36 months – has a manufacturing advantage thanks to a deal with the Serum Institute of India to produce up to 200 million doses annually.
In contrast, GSK has committed to producing up to 15 million doses of Mosquirix every year through 2028, well under the roughly 100 million doses a year of the four-dose vaccine the WHO says is needed long-term to cover around 25 million children.
Mid-stage data from the Oxford vaccine trial involving more than 400 young children was published in a medical journal in September.
Vaccine effectiveness was 80% in the group that received a higher dose of the immune-boosting adjuvant component of the vaccine, and 70% in the lower-dose adjuvant group, at 12 months following the fourth dose. The doses were administered ahead of the peak malaria season in Burkina Faso.
Data from an ongoing phase III clinical trial in Burkina Faso, Kenya, Mali, and Tanzania that has enrolled 4,800 children is expected to be published in a medical journal in the coming months.
More News: Desist from Late Night Learning – UCC Students told
However, late-stage data – which suggests a similar vaccine performance as in the phase II trial – has been shared with regulatory authorities over the last six months, Oxford scientist Adrian Hill said.
Childhood vaccines in Africa are typically paid for by international organizations such as Gavi and UNICEF after they have been backed by the World Health Organisation (WHO).
This is the first time a major vaccine has been approved first in an African country, before rich nations, Hill added, noting that it was unusual that a regulatory authority in Africa had reviewed the data quicker than the WHO.
“Particularly since COVID, African regulators have been taking a much more proactive stance, they’ve been saying…we don’t want to be last in the queue.”